Publications
Europe-wide IPSOS survey reveals expert views about fruit juice
Carrie Ruxton, PHD, registered dietitian
The renewed focus on sugar has tarnished the reputation of several foodstuffs that were once held to be healthy, such as 100% fruit juice, yogurt and breakfast cereals. While some authorities have a strict view – that all dietary sources of free sugar, whether natural or added, should be limited – others have used food-based dietary guidelines to consider the overall nutritional benefit and the place of foods in the diet.
As a natural source of sugars, containing around 8-9 g per 100 g or around 13 g in a 150 ml serving, 100% fruit juice (100% FJ) has been brought within the classification of high sugar foods by WHO1. Yet, it is a foodstuff that cannot be reformulated since 100% FJ is regulated by EU law2 and must mirror the sugar content of the original fruit source. Nor can 100% FJ contain added sugars and it is exempt from the Soft Drinks Industry Levy (sugar tax).
It was in this context that a survey was undertaken across Europe to explore how healthcare professionals (HCPs) consider the healthiness of 100% FJ and its role in the diet.

METHODS
An online quantitative survey by polling company, IPSOS, was commissioned by Fruit Juice Matters, which is co-funded by the European Fruit Juice Association, Citrus BR and three packaging companies. HCPs (GPs, paediatricians, dietitians, nutritionists) from 14 European countries were interviewed using structured questions, delivering an overall sample size of 2099 (391 dietitians/nutritionists) as shown below. The fieldwork was carried out between November and December 2017.
Results
Dietary advice The vast majority of HCPs (>80%) give advice about fruits and vegetables, with a slightly higher proportion amongst dietitians/ nutritionists, and HCPs working in Southern European countries. Of those giving advice, a third frequently offer specific guidance on 100% FJ. Nordic countries had the lowest proportion of HCPs offering advice about juice.
The types of advice on 100% FJ differed depending on the speciality. Dietitians and nutritionists were more likely to suggest ‘often’ that patients stopped or reduced 100% FJ consumption (23%) than positively recommending it (11%). In comparison, 12% of paediatricians and 7% of GPs frequently suggested a reduction/ cessation of juice consumption while 17% and 22% respectively recommended consumption.
The main reasons for recommending 100% FJ were that it is rich in nutrients, particularly vitamin C, that it contributes to fruit intake, and may offer health benefits. For those who advised against drinking 100% FJ, key concerns were the sugar content, a belief that 100% FJ would disrupt glycemic control and increase the risk of type 2 diabetes, or contribute to obesity risk.
This view conflicts with the evidence. For example, two meta- analyses of randomised controlled trials3,4 reported that consumption of 100% FJ had no significant impact on fasting blood glucose, insulin sensitivity or glycosylated haemoglobin levels. Another meta- analysis5 of prospective cohorts reported that 100% FJ consumption was unrelated to the risk of type 2 diabetes onset (RR=1.03, p=0.62). In 2015, the UK’s Scientific Advisory Committee on Nutrition6 reported no significant association between unsweetened 100% FJ consumption and body mass index, body fatness or fat distribution.
The reason for these findings may be that the glycemic index (GI) of 100% FJ is low to moderate7 – in the case of orange juice, it is 50 compared with 43 in whole oranges. A recent randomised cross-over trial8 compared the metabolic impact of a high intake of 100% orange juice with that of a sugar-sweetened beverage, finding important differences. Firstly, daylong control of blood glucose levels was superior following two weeks of daily orange juice (at intakes in excess of 1 l per day representing 20% of daily energy requirements). Secondly, daily orange juice prompted a significant reduction in blood uric acid levels due to increased excretion in urine – an effect not seen following daily consumption of the sugar-sweetened beverage. This has implications for the prevention of gout – an inflammatory condition that has been blamed on fruit and 100% FJ consumption. Further work by the same research group9 found that drinking orange juice with meals significantly reduced body fat, despite providing an additional 7700 kcal over the course of the two-week study.
100% FJ was viewed more as a ‘healthy complement’ to fruit and vegetable intake (67%) than as an ‘alternative’ to these foods (46%). This is in line with the view in several countries that one serving of 100% FJ counts towards targets for fruit and vegetable consumption. Interestingly, acceptance of the ‘alternative’ view was highest in Nordic countries which do not acknowledge 100% FJ as a portion of fruit in national dietary guidelines. Younger HCPs (under 35 years) were less likely to accept that 100% FJ is an ‘alternative’ to fruit (30% versus 49% of HCPs aged over 50 years).
Processed versus fresh
While fresh juice is typically seen as nutritionally better than packaged 100% FJ, this is not always the case. For example, in a randomised cross-over trial10, the flavanone content of processed 100% orange juice was higher than that seen in freshly squeezed orange juice (58 mg vs. 16 mg), resulting in a higher bioavailability in human subjects. In addition, carotenoids, vitamin C and folate are all bioavailable in packaged 100% orange juice11. Studies comparing orange juice with whole oranges have reported a higher bioavailability of carotenoids12 and flavanones13 in the juice, possibly due to the lower fibre content.
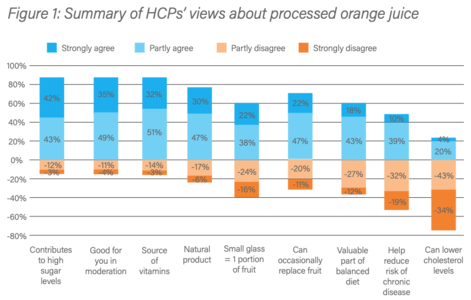
Overall, 70% of HCPs agreed that processed 100% orange juice was either very or quite good but nutritionists and dietitians held a more negative view than medics (62% agreeing). A summary of HCPs’ views about processed 100% orange juice is given in Figure 1.
Sugar
As shown in Figure 1, 85% of HCPs believe that 100% FJ contributes to high levels of sugar in the diet. While 100% FJ is clearly a source of sugar, the contribution to overall intakes is relatively modest compared with other sources, probably because average intakes are less than 100 ml daily and most people do not consume 100% FJ on most days of the week. European data suggest that 100% FJ provides 1-12% of added/free sugar in the diet14 while the UK’s National Diet and Nutrition Survey (NDNS) reported a contribution of 8% for adults and 11-14% for children (in comparison, sugar, preserves and confectionery contribute 16-25%).
A secondary analysis of the UK NDNS15 found that adults who consumed 1-150 ml of 100% FJ daily had sugar intakes of 11.9% energy compared with 10.6% in non-consumers (p<0.05). However, teenagers had similar sugar intakes (14-15% energy) regardless of whether they consumed up to 150 ml 100% FJ daily. This suggests that avoidance of 100% FJ does not lead to low sugar intakes. In the French Comportements et Consommations Alimentaires en France survey16, free sugar intakes were 11.3% of daily energy intake in 100% FJ consumers versus 8.7% in non-consumers, although juice consumers also ate more sweetened yoghurt, cakes, fruit desserts, biscuits and breakfast cereals which would have contributed significantly to sugar intakes.
In the IPSOS survey, there were strong misconceptions about the purity of orange juice. Bizarrely, given the descriptor, only 69% were sure that ‘100% orange juice’ contained just 100% orange juice, although 53% correctly said that no sugar had been added. Only 33% knew that preservatives are not added to 100% FJ. Dietitians and nutritionists had a greater degree of knowledge compared with GPs and paediatricians. Turning to bioactive compounds, only 30-40% of HCPs correctly identified that carotenoids and flavonoids were present in 100% orange juice. Again, dietitians and nutritionists were more likely to understand the nutritional composition of 100% FJ than medics.
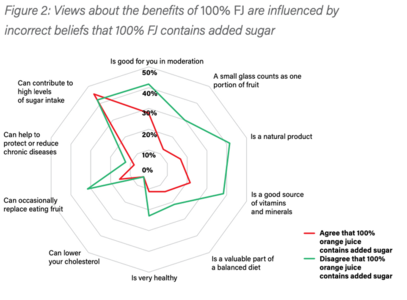
Concerns about the contribution of 100% FJ to overall sugar intakes and incorrect beliefs that 100% FJ contains added sugar tended to overshadow positive views about the potential health benefits associated with drinking moderate amounts. For example, HCPs with the strongest views on sugar were less likely to agree that 100% FJ is a good source of micronutrients, can be part of a balanced diet, or that it counts as one portion of fruit. The results of this analysis are summarised in Figure 2.
Discussion
Once a foodstuff that was actively promoted to boost vitamin C and folate intakes, fruit juice now sits under a cloud of suspicion as a consequence of the increased attention given to overall sugar intakes. While the sugars in 100% FJ have been defined as free sugars by WHO, several European countries also acknowledge that a small glass of 100% FJ can be part of a healthy, balanced diet and may count as one portion of fruit. No expert opinion to date has implicated moderate 100% FJ consumption in overconsumption of energy, or the development of obesity, cancer, or type 2 diabetes. In contrast, several randomised controlled trials support the view that 100% FJ has a neutral or positive impact on health17,18,19.
Undoubtedly, the categorisation of some natural sugars as ‘free sugars’ has influenced HCPs’ views of foodstuffs, such as 100% FJ. This may be taken a step further in the UK as Public Health England proposes to include the sugars in pureed fruit, vegetable and legume products as free sugars, such as smooth vegetable soups, hummus, extruded fruits, and tomato puree20. The revised Nutrient Profiling Model would also label 100% FJ as ‘high fat, salt, sugar’ and restrict its advertising. Yet, 100% FJ still sits within the Eatwell Guide as a portion of fruit, which could lead to some confusion.
Misconceptions about 100% FJ may also influence HCPs’ views, as more than a third were uncertain or disbelieved that 100% orange juice means that the only ingredient is orange juice. Around a half believed wrongly that sugar had been added, or were unsure, while just under seven in ten were unaware that there are no preservatives in 100% FJ. HCPs were also concerned about the glycemic impact of 100% FJ. This is in direct contrast to meta-analyses which show that juice has a similar glycemic index to whole fruit and does not adversely affect glycemic control or pose a risk of type 2 diabetes.
These misconceptions may have led to the low proportion of HCPs that recommend that patients consume 100% FJ (10% of dietitians/ nutritionists and around 20% of medics). Nevertheless, 70% of HCPs felt that processed 100% orange juice was good or very good, and most HCPs were supportive of 100% FJ being part of a balanced diet and complementing fruit intakes.
Conclusion
HCPs hold mixed views on the role of 100% FJ and its likely impact on health, perhaps driven by misconceptions. Improved knowledge about the composition of 100% FJ, particularly the lack of added sugars or preservatives, may rebalance HCPs opinions about 100% FJ. A fuller understanding of the literature on the likely metabolic effects of regular 100% FJ consumption may also help in this.
Dr Ruxton works on a freelance basis for Fruit Juice Matters to create content and advise on the scientific literature.
Disclaimer: Every effort has been made to ensure that the information contained in this document is reliable and has been verified. The information is intended for non-commercial communication to healthcare professionals only. The information given in this dossier does not constitute dietary advice.
References
1. World Health Organization (2015) Guideline: Sugars intake for adults and children. Geneva; World Health Organization. www.who.int/nutrition/ publications/guidelines/sugars_intake/en.
2. EuropeanParliamentandoftheCouncil(2012)Fruitjuice directive. http://eur-lex.europa.eu/LexUriServ/LexUriServ. do?uri=OJ:L:2012:115:0001:0011:EN:PDF.
3. Murphy MM et al. (2017) 100% Fruit juice and measures of glucose control and insulin sensitivity: a systematic review and meta-analysis of randomised controlled trials. Journal of Nutritional Science 6 (e59): 1-15.
4. Wang B et al. (2014) Effect of fruit juice on glucose control and insulin sensitivity in adults: a meta-analysis of 12 randomized controlled trials. PLoS One 9(4):e95323.
5. Xi B. et al. (2014) Intake of fruit juice and incidence of type 2 diabetes: a systematic review and meta- analysis. PLoS ONE 9: e93471.
6. SACN (2015) Carbohydrates and health. www.gov.uk/government/ publications/sacn-carbohydrates-and-health-report.
7. Atkinson RD et al. (2008) Diabetes Care 2008 Dec; 31(12): 2281-2283. http://care.diabetesjournals.org/content/31/12/2281.
8. Büsing F et al. (2018). High intake of orange juice and cola differently affects metabolic risk in healthy subjects; in: Clinical Nutrition; in press.
9. Hägele FA et al. (2018) High orange juice consumption with or in-between three meals a day differently affects energy balance in healthy subjects. Nutr Dietet 8: 19.
10. Silveira JQ et al. (2014) Pharmacokinetics of flavanone glycosides after ingestion of single doses of fresh-squeezed orange juice versus commercially processed orange juice in healthy humans. J Agric Food Chem 62: 12576-84.
11. Franke AA et al. (2005) Bioavailability and antioxidant effects of orange juice components in humans. J Agric Food Chem 53: 5170-8
12. Aschoff JK et al. (2015) Bioavailability of β-cryptoxanthin is greater from pasteurized orange juice than from fresh oranges – a randomized cross- over study. Mol Nutr Food Res 59: 1896-904.
13. Aschoff JK et al. (2016) Urinary excretion of Citrus flavanones and their major catabolites after consumption of fresh oranges and pasteurized orange juice: A randomized cross-over study. Mol Nutr Food Res 60: 2602- 2610.
14. Azaïs-Braesco V et al. (2017) A review of total & added sugar intakes and dietary sources in Europe. Nutrition Journal 16: 6.
15. Gibson S & Ruxton CHS (2016) Fruit juice consumption is associated with intakes of whole fruit and vegetables, as well as non-milk extrinsic sugars: a secondary analysis of the National Diet and Nutrition Survey. Proc Nutr Soc 75 (OCE3): E259.
16. Bellisle F et al. (2018) Consumption of 100% Pure Fruit Juice and Dietary Quality in French Adults: Analysis of a Nationally Representative Survey in the Context of the WHO Recommended Limitation of Free Sugars. Nutrients10: pii: E459.
17. Ribeiro C et al. (2017) Orange juice allied to a reduced-calorie diet results in weight loss and ameliorates obesity-related biomarkers: A randomized controlled trial. Nutrition 38:13-19.
18. Aptekmann NP & Cesar TB (2010) Orange juice improved lipid profile and blood lactate of overweight middle-aged women subjected to aerobic training. Maturitas 67: 343-7.
19. Grace KZS et al. (2015) Investigation of cytokines, oxidative stress, metabolic, and inflammatory biomarkers after orange juice consumption by normal and overweight subjects. Food & Nutrition Research 59: 28147.
20. Swan GE et al. (2018) A definition of free sugars for the UK. Pub Health Nutr; 21: 1636-1638..